Sleep is essential to mental and overall physical wellbeing, with many psychological disorders leading to poor restful slumber; research demonstrates how better restful nights may help treat them effectively.
Cross-sectional studies are effective for identifying associations but cannot establish causality. To establish this link, longitudinal designs must be utilized.
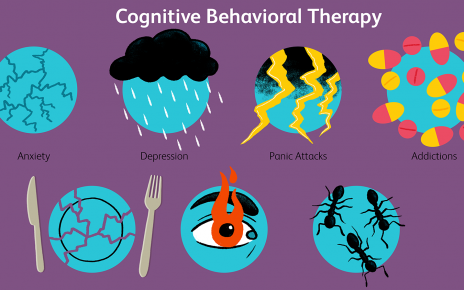
Depression
Although the exact cause remains elusive, mental health disorders often make sleeping problems worse and poor rest is an indicator of many mental conditions. For example, insomnia is a frequent side effect of depression and research suggests it could worsen or even impede its treatment.
Sleep deprivation increases the risk of psychotic disorders like schizophrenia or psychosis. Studies suggest that improving sleep could prevent or treat these conditions, including hallucinations and delusions.
Research on sleep and mental health is predominantly observational, making it challenging to draw causal inferences. Cross-sectional designs only demonstrate some correlations, while longitudinal designs allow some causal inference but remain susceptible to residual confounding. Interventionist approaches that experiment with manipulating sleep are necessary in order to verify whether changes lead to improvements in mental health outcomes; additionally, studies comparing groups with and without similar interventions help reduce impact due to confounds.
Anxiety
Sleep problems are one of the primary complaints reported to mental health professionals, and are increasingly thought to both increase risk for and directly worsen some psychiatric conditions, including depression and anxiety. Because this relationship runs both ways, research into its nature must continue in this area.
Studies that evaluate the effects of interventions that improve sleep on various mental health outcomes are urgently required. For optimal research results, designs with low risk of bias should be employed for causal inference purposes, including longitudinal and randomized controlled trials.
Additionally, the effects of sleep interventions on mental health should be evaluated across populations, settings and study designs. Furthermore, variables that moderate (moderator tests using both categorical and continuous variables) the impact of interventions should also be explored; results of such analyses would inform future research and practice activities such as age, gender, comorbid conditions and sleep quality as potential moderators of such effects.
Bipolar Disorder
Sleep problems have often been seen as symptoms of mental health disorders like depression or anxiety; however, research indicates that poor sleeping patterns could actually increase risk and contribute to developing certain psychiatric conditions directly.
One study discovered that individuals living with bipolar disorder experience increased risks of depression and delusional thinking when experiencing insomnia, according to one research paper from University of Maryland School of Medicine (UMSOM). Furthermore, UMSOM also published another recent research paper showing children sleeping less than nine hours each night had significantly smaller brain volume in areas responsible for mood regulation, memory storage and impulse control than those receiving nine or more hours’ rest each night.
Randomised controlled trials have demonstrated the link between interventions to improve sleep and mental health and long-term follow up studies; most do not report long-term follow up and high risk of methodological bias; long-term follow up studies will help to establish whether benefits of improved sleep persist over time and to examine possible mechanisms.
Schizophrenia
Mental health difficulties are all too familiar and can have profound effects on one’s life. Sleep aid isn’t a panacea for mental illness, but it may help minimize its symptoms as part of any treatment plan.
Insomnia can be an enormously challenging issue for those living with schizophrenia or other mental disorders, making treatment plans harder to adhere to and increasing the risk of mental health episodes or recurrences. Furthermore, insomnia can contribute to psychotic episodes such as hallucinations.
Studies demonstrate the relationship between interventions to enhance sleep and mental health difficulties. One study demonstrated this correlation by finding that better sleeping reduced depression, anxiety, stress and suicidal thoughts while another discovered it reduced psychotic symptoms and enhanced mood. For people living with schizophrenia or bipolar disorder improving sleep may help increase response to their medications more quickly.